Numerous studies have demonstrated the potential efficacy of CT-guided percutaneous needle-based therapy and biopsy in a wide variety of medical problems. Contemporary practice, however, is limited by the freehand technique, which requires mental registration of the patient’s anatomy to the CT image in targeting and precise hand-eye coordination in inserting the needle. This often leads to faulty needle placement attempts followed by repeated CT scans and adjustments, increasing the discomfort and radiation exposure of the patient and lengthening the procedure. Practitioners generally agree that, given enough time and opportunity for intermittent CT imaging and adjustments, the target usually can be reached with appropriate accuracy. The important question is, however, whether the same objective could be achieved with just one attempt, because each correction requires taking an extra CT image (or even series of images) and reinsertion of the needle, which in turn increases the risk of post-procedure complication, discomfort, and radiation exposure to the patient. Therefore, eliminating faulty needle insertion attempts is a prime objective of our research.
Project Overview
|
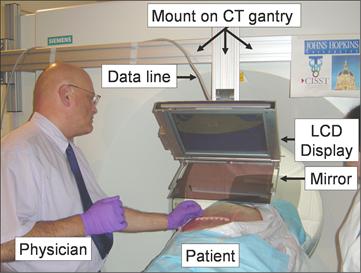
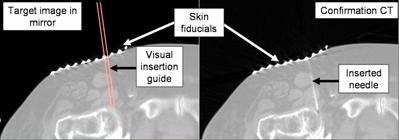
Numerous studies have demonstrated the potential efficacy of CT-guided percutaneous needle-based therapy and biopsy in a wide variety of medical problems. Contemporary practice, however, is limited by the freehand technique, which requires mental registration of the patient’s anatomy to the CT image in targeting and precise hand-eye coordination in inserting the needle. This often leads to faulty needle placement attempts followed by repeated CT scans and adjustments, increasing the discomfort and radiation exposure of the patient and lengthening the procedure. Practitioners generally agree that, given enough time and opportunity for intermittent CT imaging and adjustments, the target usually can be reached with appropriate accuracy. The important question is, however, whether the same objective could be achieved with just one attempt, because each correction requires taking an extra CT image (or even series of images) and reinsertion of the needle, which in turn increases the risk of post-procedure complication, discomfort, and radiation exposure to the patient. Therefore, eliminating faulty needle insertion attempts is a prime objective of our research. Perhaps the most important element of principle is that we do not project the CT image into the surgical field, we merely make it appear there, hence the name “virtual reality” display. The central piece of the system is a half-mirror, which has two useful properties: one can see through the half-mirror and see the scene behind it, while at the same time one can also see reflections in the half-mirror. The reflections are fainter than they would be in a full mirror and the transparent scene is also fainter than it would be through clear glass, but with proper lighting, a reasonable compromise can be achieved between the two. The overall concept is as simple as this: acquire a CT slice, render the image on a distortion-free flat panel display and position the display above the half mirror, so that the reflection of the CT slice coincide with the patient’s body that we see behind the mirror. This system results in an optically stable alignment of the real view and the image in the mirror, provided that the mirror, the display and the scanner were properly aligned earlier. The key questions are how to build a system like this, which is also lightweight, inexpensive, easy to setup, easy to calibrate, independent from the actual CT scanner, and ergonomic to both patient and physician.
Click here to see an MPEG video clip of the system in action in a phantom experiment. |
Driving Clinical Applications
 We propose to demonstrate the advantages of CT image overlay first in musculoskeletal (MSK) biopsy. Skeletal neoplasms, especially metastatic cancers are common causes of bone destruction in adult patients. In the evaluation of musculoskeletal neoplasms, the first objective is diagnosis, followed by alleviation of pain and prevention of complications, such as pathologic fractures. Accurate assessment of the disease is vital for deciding on the appropriate treatment. Percutaneous needle biopsy of bone and soft tissue tumors is rapidly gaining popularity as the standard of care in the assessment of musculoskeletal tumors. The benefits of this procedure include cost efficiency, patient convenience, and avoidance of complications associated with the open biopsy technique that was the original method of obtaining histologic diagnoses. Accuracy rates for percutaneous core-needle biopsy are as high as 100% for metastatic disease, although they may be as low as 59%, depending on the nature of the lesions (i.e., whether sclerotic or lytic), their histology, and site within the body. This type of biopsy is, nevertheless, considered a logical, effective tool in the diagnosis of bone and soft tissue tumors, given that open biopsies carry potentials for significant complications. Generally, percutaneous core-needle biopsy has been found to be an effective alternative to open biopsy in the evaluation of possible neoplasms of bone or soft tissue. We propose to demonstrate the advantages of CT image overlay first in musculoskeletal (MSK) biopsy. Skeletal neoplasms, especially metastatic cancers are common causes of bone destruction in adult patients. In the evaluation of musculoskeletal neoplasms, the first objective is diagnosis, followed by alleviation of pain and prevention of complications, such as pathologic fractures. Accurate assessment of the disease is vital for deciding on the appropriate treatment. Percutaneous needle biopsy of bone and soft tissue tumors is rapidly gaining popularity as the standard of care in the assessment of musculoskeletal tumors. The benefits of this procedure include cost efficiency, patient convenience, and avoidance of complications associated with the open biopsy technique that was the original method of obtaining histologic diagnoses. Accuracy rates for percutaneous core-needle biopsy are as high as 100% for metastatic disease, although they may be as low as 59%, depending on the nature of the lesions (i.e., whether sclerotic or lytic), their histology, and site within the body. This type of biopsy is, nevertheless, considered a logical, effective tool in the diagnosis of bone and soft tissue tumors, given that open biopsies carry potentials for significant complications. Generally, percutaneous core-needle biopsy has been found to be an effective alternative to open biopsy in the evaluation of possible neoplasms of bone or soft tissue. |
|
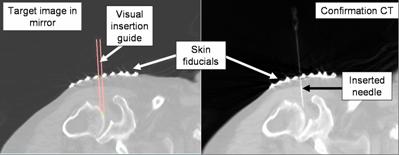
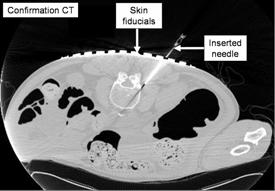
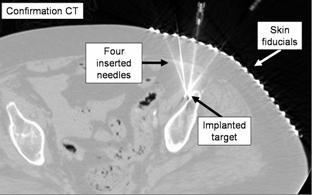
Another clinical application in which we propose to demonstrate the advantages of CT image overlay is joint arthrography. CT-guided arthrography is one of many potential CT-guided interventional procedures performed in the musculoskeletal system [Binkert-2003]. Joint arthrography is performed in a growing number of cases and provides a minimally-invasive method for the detection of ligamentous, tendon and fibrocartilage injury in joints. Its sensitivity and specificity for these abnormalities is variable, depending on the joint and imaging modality used. While MRI is generally more popular, in certain conditions CT offers an excellent alternative. Most often, CT provides guidance for direct injection of gadolinium into a joint to be used in subsequent MRI imaging to assess the condition of the joint. In these cases CT is applied generally the same way as fluoroscopic guidance is used for gadolinium injection. A comparative study found that CT-guided injection of joints was equally accurate and yielded slightly decreased examination times compared with fluoroscopy guidance. While conventional C-arm fluoroscopy remains the popular modality for arthrographic contrast injection due to the ease and availability of fluoroscopic units, CT guided injection is also accurate, simple, fast, and effective; and it can be recommended when a CT is available.
Target and confirmation CT for the arthography of shoulder (top) and hip joint (bottom), in human cadaver |
|
Spinal disorders are undoubtedly the fastest growing musculoskeletal subspecialty, consuming an estimated $120 billion dollars for direct and indirect costs. The acceleration in the number of new cases treated annually reflects the aging of our society as well as the dramatic transformation of the traditional workplace into offices that impose extreme stress on the skeletal system, primarily on the spine. It is estimated that over 70% of our population experiences significant low-back pain, with 10% reporting sciatica and 1% requiring long-term conservative and/or surgical intervention. Minimally invasive percutaneous pain management in the spine has gained a lot of interest lately. CT-guided nerve blocks and facet joint injections have proven to be safe and effective methods to alleviate severe pain and provide longstanding relief for patients of all age and sex. Typically, these procedures require a single puncture with a thin needle across the superficial soft tissue, and the use of a multiple CT images for confirmation of the needle position as it is advanced. However simple and easy these procedures may appear, there is great need for precise and consistent aiming and delivery of the needle. The longevity of pain relief is thought to be associated with the spatial accuracy of needle placement. Even these single-puncture procedures present large variability from surgeon to surgeon. For example, the length of the procedure varies between 10 and 45 minutes, depending on the experience of the interventionalist. Longer times are usually associated with occasional misplacement of the needle, often several times, before its correct position is confirmed. Misplacements also include over-pushing the needle, which causes sharp pain to the patient and must be avoided at all cost. Very importantly, misplacement of the needle necessitates extra CT images, each time exposing the patient to unnecessary toxic radiation. |